Psilocybin research opportunities in the United States are expanding under a clear federal framework for controlled substance studies. Institutions can conduct preclinical and clinical work through the existing FDA and DEA pathways with the right approvals, documented supply, and trained teams. The current climate favors projects that pair strong trial design with reliable product quality and transparent reporting.
Current research climate in the U.S.
Interest in psilocybin has grown across universities, hospitals, and private labs. The field draws from psychiatry, neurology, pharmacology, and outcomes research. Programs recruit experienced investigators, independent ethics boards, and specialty CROs. Many centers already have processes for handling Schedule I substances and can adapt those systems for psilocybin.
Sponsors now plan studies that track symptom change, function, and relapse over longer windows. This shift adds weight to durability questions and supports payer discussions later. As designs mature, reviewers expect careful handling of therapy variables, such as preparation visits, dosing day setting, and integration follow up. These protocol elements affect both efficacy and safety, so teams document them in detail.
Stakeholders also focus on standardization. Method papers and interlab comparisons have improved agreement on psilocybin and psilocin assays. Sponsors share stability data that fit real site storage and transport conditions. These steps improve confidence in dosing accuracy and reduce hold points during pharmacy intake.
Funding flows from multiple sources. Philanthropy supports centers of excellence and training. Venture and public markets fund drug developers. Federal grants back basic science and some clinical pilots. This mix supports a pipeline from mechanism to larger trials and expands the market for validated testing, data tools, and site services.
Federal scheduling and permitted uses
Psilocybin is a Schedule I substance under federal law. That status shapes, but does not block, research. Work proceeds under FDA and DEA oversight with institution and investigator controls in place.
Permitted uses for research include
- Preclinical studies under controlled laboratory conditions
- Phase 1 studies in healthy volunteers with safety as the main aim
- Phase 2 and Phase 3 studies in patient populations with defined endpoints
- Human factors, storage, and pharmacy handling studies that support clinical use
Key federal elements include
- An active IND or an accepted pathway for the proposed human study
- A DEA registration for the site and for any location that will store or dispense study drug
- Source documentation that proves lawful manufacture or export and a legal import into the U.S.
- Chain of custody from supplier to site with matching labels and records
- IRB approval that covers all visits, consent, and data handling
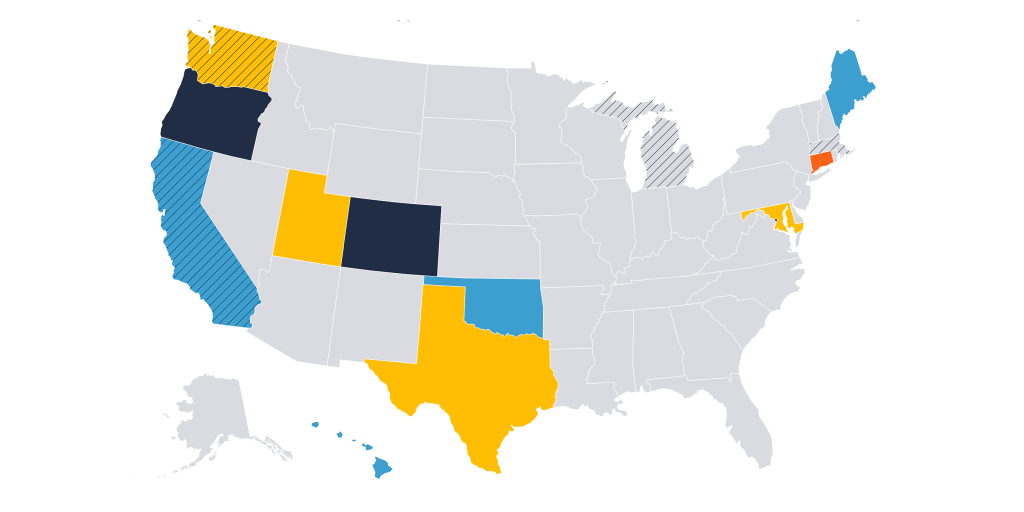
These controls apply in every state. Local rules may add steps, but the federal path sets the core. Teams that build clean document packages move faster through startup and avoid shipment delays.
Active areas of investigation
Depression
Major depressive disorder and treatment resistant depression remain central. Trials assess single session and multiple session designs, often paired with structured therapy. Endpoints include response, remission, and functional measures across weeks and months. Safety tracking covers cardiovascular status, suicidality, and treatment emergent adverse events. Studies also test different dose levels and visit schedules to find plans that balance effect size, safety, and site capacity.
Post traumatic stress disorder
PTSD programs adapt trauma focused therapy into the dosing framework. Investigators watch for dissociation, anxiety spikes, and sleep effects. They train teams to handle difficult sessions with calm, consistent methods. Endpoints include clinician rated scales, self report measures, and quality of life. Sponsors publish therapy manuals and supervision plans to hold fidelity across centers.
Substance use disorders
Alcohol and tobacco use disorders are common targets. Designs track craving, use days, and biochemical checks. Programs often include motivational work and support visits before and after dosing. Longer follow up windows help quantify durability and relapse patterns. Sites build referral links to community care so participants can access support after study end.
Anxiety and end of life distress
Patients facing serious illness may benefit from focused protocols with careful screening and medical oversight. Teams coordinate with oncology, palliative care, or specialty clinics. Safety planning covers drug interactions, vital sign monitoring, and rapid response steps. These trials often weigh outcomes tied to meaning, mood, and fear with respected instruments.
Headache and pain
Smaller programs explore cluster headache and certain pain conditions. These studies require tight diagnostic criteria and close safety review. Dosing plans and endpoints are tailored to each condition, and pharmacy teams focus on timing and adherence.
Across all areas, sponsors report more process data. Reviewers want to see deviation rates, reasons for withdrawal, adherence to visit windows, and how sites handled blind protection. These signals strengthen confidence in the readout and support design choices in the next phase.
Why research grade psilocybin supply is essential
Research grade supply holds trials together. Accuracy, stability, and traceability affect every step from import to last visit. A strong supply program does five things well.
- Documents every transfer
Each carton, kit, and vial matches a record with lot, label, and quantity. Chain of custody links the supplier to the site pharmacy. Discrepancies trigger investigations with clear closeouts. - Proves identity and strength
Certificates of analysis list psilocybin, psilocin, and key impurities with pass limits. Methods reference validated procedures. Results tie to the exact lot and container type. - Shows stability under real conditions
Reports cover long term and accelerated storage with temperatures that match site refrigerators and freezers. Transport studies cover time out of storage during shipment and receipt. - Aligns with interlab checks
Suppliers and independent labs run comparison studies. Acceptable ranges and pass criteria are set in advance. Results reduce disputes and speed intake. - Supports kit design and blind integrity
Labels, kit maps, and pharmacy instructions protect allocation. Placebo design is documented. Sites receive the same layouts and drill scripts, which reduces error.
As suppliers, we align kit maps, label sets, and shipment records with hospital workflows, then join mock intake to confirm that receiving steps match documents and cartons. That lowers the risk of intake holds and keeps first dose on schedule.
Storage and pharmacy setup
Hospital pharmacies set controlled access, temperature monitoring, and log review. They train staff who handle receiving, preparation, and dispensing. They test alarm responses and backup power. Sites keep records for all checks and signoffs. A well planned intake prevents delays at site activation.
Therapy and site readiness
Dosing days rely on trained teams and prepared rooms. Therapy supervisors cover key roles and visit scheduling. Session rooms meet safety and privacy needs. Teams document preparation visits and keep device use limited to what the protocol allows. These steps support clean data and a safe participant experience.
Regulatory readiness
Import packets, DEA forms, and IRB letters must match the product, labels, and storage plan. When files align, shipments clear faster and audits run smoothly. When they do not, sites can lose weeks at startup.
Where institutions can start
Institutions can follow a simple path to build programs that move from idea to dosing with fewer stops.
Step 1 set the scope
- Define indication, endpoints, and follow up windows
- Choose single site or multisite
- Decide on single session or multiple session design
- Draft a realistic enrollment plan that matches local capacity
Step 2 map the controls
- Confirm DEA registration and storage readiness for each site
- Select an IRB with controlled substance experience
- Identify therapy leads and set supervision schedules
- Select a supplier with documented import history, COAs, and stability data
- Align on dose form, strength, and kit design
Step 3 build the file set
- Prepare the IND or applicable submission with clear rationale and safety plan
- Assemble consent forms, manuals, pharmacy SOPs, and chain of custody templates
- Pre draft import requests and site receiving checklists
- Create deviation handling plans and data safety board charters
Step 4 rehearse the workflow
- Run mock receiving at the pharmacy with real labels and blank cartons
- Conduct dry runs of preparation visits and dosing day steps
- Verify temperature logs, alarms, and backup power
- Test eCRFs for time stamps, queries, and export formats
Step 5 launch and monitor
- Track site startup cycle times and remove bottlenecks
- Watch visit window adherence and dropout reasons in real time
- Share safety signals with monitors and the board on a set cadence
- Keep interlab checks and stability reviews on schedule
Early projects that build capability
Institutions that are new to this space can start with pilots that strengthen teams and files.
- Small Phase 1 studies in healthy volunteers with careful safety windows
- Method validation projects that compare assay results across labs
- Storage and handling studies that mirror local conditions
- Training cohorts for therapy staff with supervision records
These efforts build momentum and reduce risk before larger patient trials.
Closing opportunities and next steps
Psilocybin research in the United States has clear paths for legal supply, documented handling, and rigorous trial conduct. The largest opportunities sit in programs that match strong clinical questions with careful operations. Depression, PTSD, and addiction remain high value areas. Hospitals that build pharmacy controls and therapy depth will be ready for larger studies. Suppliers that share clean records and support intake help sites dose on time and protect the blind.
Institutions can start by setting scope, mapping controls, and building a solid file set. Rehearsals at the pharmacy and in session rooms reveal gaps before first shipment. Early pilots build staff skill and shorten startup on larger trials. With that foundation, teams can run studies that answer pressing questions and hold up under review.